Microaggressions matter for Queer health justice
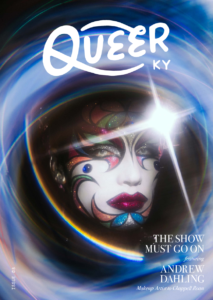
This article is a part of Queer Kentucky ISSUE 02 where we explore how community and connection benefit the health of LGBTQ+ Kentuckians. You can purchase here.
By now, the term “microaggression” is quite common and many people have a general sense of what microaggressions are – especially if they find themselves on the constant receiving end of them. Among researchers who study the phenomenon, microaggressions are typically defined as frequent and seemingly subtle insults, slights, dismissals, or snubs, which communicate bias or hostility to someone on the basis of one or more marginalized identities that they hold.
Though microaggressions can seem like minor and often unintentional “mistakes” from the perspective of those committing them, they can be deeply harmful for those who are on the constant receiving end of microaggressive comments and actions.
LGBTQ+ people are susceptible to microaggressions in all walks of life, given the persistent stigma against LGBTQ+ identities and experiences. Though microaggressions can be detrimental in any and all contexts in which they occur, they can be especially harmful when they occur in healthcare settings. This is because healthcare contexts are especially prone to power imbalances, since patients, especially patients from marginalized groups, are often in vulnerable states when seeking treatment or care. This is especially true in our current sociopolitical context, in which LGBTQ+ people are seeking health care against the backdrop of legislative attacks on their communities, identities, and their very ability to access what can be lifesaving care.
In medical contexts, microaggressions against LGBTQ+ are common, though they might go unnoticed by cisgender/heterosexual providers, staff, and patients. Consider some examples:
- Patient intake forms often exclude gender-inclusive options for sex and genderidentification (thereby erasing trans, non-binary, and intersex people).
- Clinic staff and practitioners often misgender or deadname trans and non-binary patients.
- Non-heterosexual and non-monogamous people often face questions about sexual behavior that presuppose heterosexuality and monogamy.
- Medical brochures and information sheets are often written in a way that exclusively refers to binary gender identity and heterosexual sexual experience.
- Queer and trans patients are often asked irrelevant questions about their gender identities, physical bodies, or sexual behavior when those things have no bearing on the issue at hand.
These are just a few examples, though similar examples abound, and LGBTQ+ people know them all too well. Though these types of microaggressions and others often occur without malicious intent, they can cause deep harm making LGBTQ+ patients feel like they aren’t being seen, heard, or understood in the ways they deserve to be. And this is important, because feeling as if one is being listened to, understood, and respected are all necessary conditions for the kinds of trust, openness, and communication that quality healthcare requires.
Without these conditions, LGBTQ+ people can be further pushed out of healthcare spaces, and may avoid or delay seeking
critically important care. Minimizing the microaggressions that LGBTQ+ people face when interacting with healthcare institutions is imperative as a matter of health justice. LGBTQ+ people deserve to be seen and treated with respect in all settings, but especially in settings in which their health, well-being, and even lives depend on the ability to trust and be open with their providers.
So, how can healthcare clinics create spaces that foster a genuinely inclusive healthcare environment for LGBTQ+ patients beyond simply engaging in performative allyship? To do so requires fostering a genuine sense of belonging for LGTBQ+ patients – that is, a feeling of being recognized, taken seriously, and respected by all people in the clinical space. Here are some tips for doing so:
- Soliciting names and pronouns on intake forms and then using them consistently.
- Identifying one’s own pronouns (e.g., having them on staff and provider name badges).
- Having inclusive language and imagery on medical information sheets, pamphlets, and posters.
- Avoiding unnecessary and invasive questioning when it is not directly relevant (and when it is relevant, using care to ensure that these issues are approached with due sensitivity).
- Soliciting input from local queer health advocates about how to be more inclusive (and compensating such advocates for their time and expertise).
- Advocating for diverse hiring practices to ensure that there is diverse representation among clinic staff at all levels.
- Advocating for LGBTQ+ patients beyond the clinic – showing up for LGBTQ+ people and communities socially and politically, and being aware of how structural inequalities influence health outcomes.
Though these tips are not perfect, nor are they complete, they offer an important starting place. Those who are tasked with the responsibility of providing care to anyone, and especially to the people and communities society already renders vulnerable in far too many ways, must take every step possible to avoid any preventable harm, and to promote justice at any and all costs.