Kentucky House Bill 553 bill could strip insurance coverage for gender-affirming care from thousands
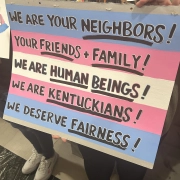
Access to gender-affirming health care for LGBTQ+ Kentuckians may be further restricted under a new bill filed Tuesday.
A 2025 law in Kentucky prohibited Medicaid dollars from covering gender-affirming hormone treatments and surgeries. This year’s House Bill 553, filed by Republican Rep. Josh Calloway, seeks to expand those restrictions to most taxpayer-funded health plans and to far more services.
If passed as written, that would mean those on state and local government employee health plans, those working at public colleges and universities, KCHIP and Medicaid, and more, would no longer be able to have such services covered under their health insurance.
HB 553 also uses a much more broad definition of what counts as a “gender transition service,” blocking basically every “surgical, medical, mental health, or pharmaceutical” service “performed for the purpose of altering the appearance of an individual’s sex or validating or affirming an individual’s perception of the individual’s sex, if that appearance or perception is inconsistent with the individual’s sex.”
This includes any drug and any sort of counseling or therapy, the bill says.
There are specific carveouts for intersex people and those who wish to detransition.
The bill also would require licensing boards for health care providers to revoke providers’ licenses if found to be in violation of the law, and prohibits resource centers in schools from giving referrals for gender transition services.
As of Tuesday night, an impact statement examining exactly how many people tied to state-level health plans the bill could impact and any potential savings or extra costs could result from the bill was still being prepared.
Calloway filed a similar bill last year, but it never got a committee hearing — the first big step in the legislative process for House bills.